Nursing Care Plan For an Unconscious Patient – In this article, we’ll explore the Unconscious causes, diagnosis, and management of an unconscious patient, and what you can do to provide the best possible care through a Nursing Care Plan for an Unconscious Patient.
Unconscious Patient Definition
An unconscious patient is someone who is not aware of their surroundings, cannot communicate, and is unable to respond to stimuli. It can be a very scary situation for both the patient and their loved ones. However, with the right care and support, an unconscious patient can recover and return to their normal life.
Causes of Unconsciousness:
Unconsciousness can be caused by a variety of factors, including:
- Traumatic brain injury
- Stroke
- Seizures
- Infections
- Toxins or poisons
- Heart attack or cardiac arrest
Nursing Care Plan For an Unconscious Patient
The nursing care plan for an unconscious patient may vary depending on the patient’s underlying condition and the healthcare provider’s instructions. It is important to follow an individualized plan of care for each patient.
Nursing assessment of unconscious patient
Assessing an unconscious patient can be a challenging task for a nurse. However, a thorough nursing assessment is critical to identify any changes in the patient’s condition, monitor vital signs, and identify potential complications. Here are the key areas to focus on when assessing an unconscious patient:
- Airway:
The nurse should assess the patient’s airway for any signs of obstruction or compromise. This may involve monitoring the patient’s breathing rate, assessing for the presence of stridor or wheezing, and monitoring for any signs of respiratory distress.
- Breathing:
The nurse should assess the patient’s breathing pattern and respiratory effort. This may involve monitoring the patient’s respiratory rate, rhythm, and depth, as well as assessing for any signs of apnea, hypoventilation, or hyperventilation.
- Circulation:
The nurse should assess the patient’s cardiovascular system, including blood pressure, heart rate, and rhythm. This may involve monitoring for any signs of hypotension or hypertension, tachycardia or bradycardia, and irregular heart rhythms.
- Neurological status:
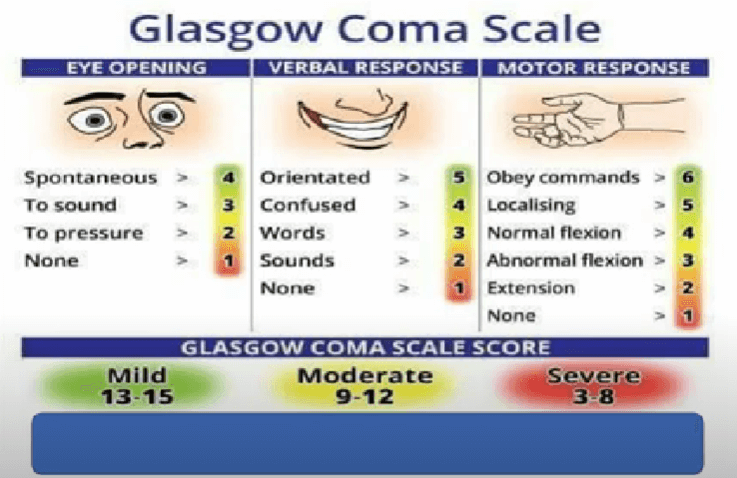
The nurse should assess the patient’s level of consciousness using a tool such as the Glasgow Coma Scale (GCS) or other appropriate tools. This may involve assessing the patient’s response to verbal and physical stimuli, as well as monitoring for any signs of changes in mental status.
- Skin:
The nurse should assess the patient’s skin for any signs of pressure ulcers, skin breakdown, or other skin conditions. This may involve assessing the patient’s skin color, temperature, and moisture level, as well as monitoring for any signs of skin irritation or breakdown.
- Hydration and Nutrition:
The nurse should assess the patient’s hydration status and nutritional needs. This may involve monitoring the patient’s intake and output, as well as assessing for any signs of dehydration or malnutrition.
- Urinary and bowel function:
The nurse should assess the patient’s urinary and bowel function, including monitoring for any signs of urinary retention, urinary incontinence, constipation or diarrhea.
- Emotional support:
The nurse should also assess the patient’s emotional well-being and provide support and reassurance to the patient and their family members.

In summary, assessing an unconscious patient requires a thorough and systematic approach that addresses all aspects of the patient’s condition. By focusing on these key areas, the nurse can identify any changes in the patient’s condition, monitor vital signs, and provide appropriate interventions to promote the patient’s recovery.
10 nursing diagnoses for an unconscious patient
Nursing diagnosis for an unconscious patient may vary depending on the patient’s underlying condition and clinical manifestations. Here are ten possible nursing diagnoses for an unconscious patient:
- Risk for aspiration related to a decreased level of consciousness and impaired cough reflex.
- Risk for impaired skin integrity related to immobility and prolonged pressure.
- Risk for ineffective cerebral tissue perfusion related to altered level of consciousness and decreased cerebral blood flow.
- Risk for impaired oral mucous membrane related to decreased oral intake and dehydration.
- Impaired gas exchange is related to a decreased level of consciousness and ineffective cough.
- Risk for infection related to invasive devices and impaired immune response.
- Risk for injury related to a decreased level of consciousness and environmental hazards.
- Impaired urinary elimination is related to a decreased level of consciousness and urinary retention.
- Imbalanced nutrition: less than body requirements related to decreased oral intake and impaired swallowing.
- Anxiety related to altered level of consciousness and unfamiliar environment.
Planning:
- Maintain a patent airway and prevent aspiration by elevating the head of the bed, suctioning secretions, and providing oral care.
- Promote skin integrity by repositioning the patient every 2 hours, using pressure-relieving devices, and providing skin care.
- Monitor the patient’s cerebral perfusion by maintaining a stable head position, monitoring blood pressure, and providing adequate oxygenation.
- Provide oral care to prevent dry mouth, mucosal irritation, and infection.
Interventions:
- Position the patient correctly to maintain a patent airway and prevent aspiration.
- Suction secretions and provide oral care every 2 hours.
- Reposition the patient every 2 hours to prevent pressure ulcers.
- Use pressure-relieving devices as indicated.
- Monitor blood pressure and provide oxygenation as needed.
- Provide adequate hydration and nutrition, including enteral or parenteral feeding as needed.
- Provide emotional support to the patient and their family.
Nursing interventions that are needed for unconscious patients
Here are some specific nursing interventions that are needed for unconscious patients:
- Maintain a patent airway. This is the most important intervention for unconscious patients, as it ensures that they can breathe. The nurse should position the patient’s head and neck in a neutral position, and suction the airway as needed. If the patient is not breathing on their own, the nurse may need to provide artificial ventilation.
- Prevent aspiration. Unconscious patients are at risk of aspirating their own secretions or vomit. The nurse should keep the head of the bed elevated, and suction the airway frequently. The nurse should also avoid giving the patient anything by mouth, unless specifically instructed to do so by the doctor.
- Promote skin integrity. Unconscious patients are at risk of developing pressure ulcers, as they are unable to move around and change positions on their own. The nurse should assess the patient’s skin regularly for signs of pressure ulcers, and reposition the patient every 2 hours. The nurse should also use pressure-reducing mattresses and cushions to help prevent pressure ulcers.
- Manage pain. Unconscious patients may still feel pain, even though they are unable to express it. The nurse should assess the patient’s pain regularly, and administer pain medication as needed. The nurse should also try to minimize the patient’s pain by providing comfort measures, such as positioning the patient in a comfortable position and applying warm compresses.
- Provide emotional support. Unconscious patients may not be able to communicate with their loved ones, but they can still sense their presence. The nurse should encourage the patient’s loved ones to stay with them and provide emotional support. The nurse can also help the patient’s loved ones to understand the patient’s condition and treatment plan.
These are just some of the specific nursing interventions that are needed for unconscious patients. The specific interventions that are needed will vary depending on the patient’s individual needs
Evaluation:
- The patient’s airway remains patent and there is no evidence of aspiration.
- The patient’s skin remains intact and there is no evidence of pressure ulcers.
- The patient’s cerebral perfusion is stable and there is no evidence of complications.
- The patient’s oral mucous membranes remain moist and there is no evidence of infection or irritation.
Note: The nursing care plan for an unconscious patient may vary depending on the patient’s underlying condition and the healthcare provider’s instructions. It is important to follow an individualized plan of care for each patient.
[hurrytimer id=”7390″]
FAQ Nursing Care plan For an Unconscious Patient
What is a nursing care plan for an unconscious patient?
A nursing care plan for an unconscious patient is a document that outlines the nursing interventions and care that a patient will receive while they are unconscious. It is developed based on the patient’s individual needs and their underlying condition, and it is used to guide the care provided by the nursing team.
What are the components of a nursing care plan for an unconscious patient?
The components of a nursing care plan for an unconscious patient include the patient’s diagnosis, the nursing diagnoses, the expected outcomes, and the nursing interventions. The nursing interventions may include monitoring vital signs, maintaining a patent airway, administering medications, preventing complications such as pressure ulcers, and providing emotional support.
Why is a nursing care plan important for an unconscious patient?
A nursing care plan is important for an unconscious patient because it provides a roadmap for the nursing care that the patient will receive. It ensures that the nursing care is individualized and appropriate to the patient’s needs and helps to prevent complications and improve outcomes.
Who develops a nursing care plan for an unconscious patient?
A nursing care plan for an unconscious patient is typically developed by the nursing team in collaboration with the healthcare providers and the patient’s family members. The nursing care plan is reviewed and updated regularly to ensure that it remains appropriate to the patient’s changing needs and condition.
How often is a nursing care plan reviewed for an unconscious patient?
The nursing care plan for an unconscious patient is reviewed and updated regularly, typically every shift or at least once per day. This allows for adjustments to be made based on the patient’s changing condition and ensures that the nursing care remains appropriate and effective.
Sources
- American Association of Critical-Care Nurses
- Johns Hopkins Medicine
- National Institutes of Health
READ ALSO OTHER CARE PLANS

Can you send me the nursing care plan for an unconscious patient in pdf
now we add button for download every article pdf