Nursing Management of Pain-Assessment of Pain, Multimodal Approach to Pain Management, Individualized Pain Management Plans, Individualized Pain Management Plans, Patient Education, Documentation, and Evaluation.Red Flag Exclusion Criteria of Pain
Nursing management of pain
Pain is a complex and subjective experience that affects individuals physically, emotionally, and psychologically. As nurses, we have a crucial role in the management of pain in our patients. Effective pain management not only helps alleviate suffering but also improves overall health outcomes, including reducing the risk of complications, improving quality of life, and enhancing patient satisfaction.
The effectiveness and Nursing management of pain include the following:
Assessment of Pain
Assessment is the first step in managing pain effectively. It’s important to assess the patient’s pain intensity, location, and duration, as well as the nature of the pain (e.g., sharp, dull, burning). Other important factors to assess include the patient’s emotional state, past pain experiences, and any potential contributing factors. Pain assessment tools, such as numerical rating scales or visual analog scales, can help quantify pain intensity and monitor pain over time.
Multimodal Approach to Pain Management
Pain management should be approached from a multimodal perspective, using a combination of non-pharmacologic and pharmacologic interventions. Non-pharmacologic interventions include modalities such as heat or cold therapy, massage, and relaxation techniques. Pharmacologic interventions include a range of medications, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and adjuvant drugs such as antidepressants or anticonvulsants. Using a combination of these interventions can help maximize pain relief while minimizing side effects.
Individualized Pain Management Plans
Pain management should be individualized to each patient’s unique needs and preferences. Nurses should work closely with the patient and healthcare team to develop a pain management plan that considers the patient’s pain history, medical history, and current health status. The plan should also take into account the patient’s cultural and spiritual beliefs, as these can influence pain perception and response to pain management interventions.
Patient Education
Patient education is an essential component of effective pain management. Patients should be informed about their pain management plan, including the purpose and potential side effects of any medications, as well as non-pharmacologic interventions that may be helpful. Patients should also be advised to report any changes in their pain or side effects to the healthcare team promptly. Additionally, patients should be educated about the importance of adhering to their pain management plan and reporting any changes in their pain or side effects to the healthcare team.
Documentation and Evaluation
Finally, nurses should ensure accurate documentation of pain assessment, interventions, and patient responses. Documentation should be timely and include detailed information about the patient’s pain, the interventions used, and the patient’s response. Regular evaluation of the effectiveness of pain management interventions is also critical to determine whether adjustments to the plan are needed
Red Flag Exclusion Criteria of Pain
- Child at risk of significant harm
- Suspected non-accidental injury
- Unplanned repeat ED presentation
- Infant <6 months. Pain score ≥7
- Chest pain
- Abdominal pain
- History of workplace injury
- Yellow or Red Zones observations
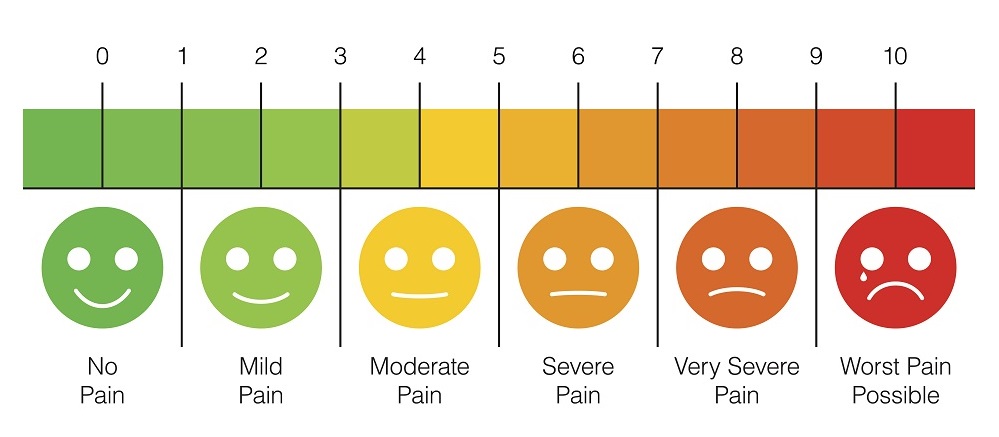
The numerical rating score of pain
Appropriate for patients aged 6-8 years and over Ask the patient to rate pain on scale below (either verbal or point on scale)
Pain Score Severity
- No pain = Pain Score of 0
- Mild pain Pain Score of 1-3
- Moderate pain= Pain Score of 4-6
- Severe pain Pain Score Above 6 (Red Flag)
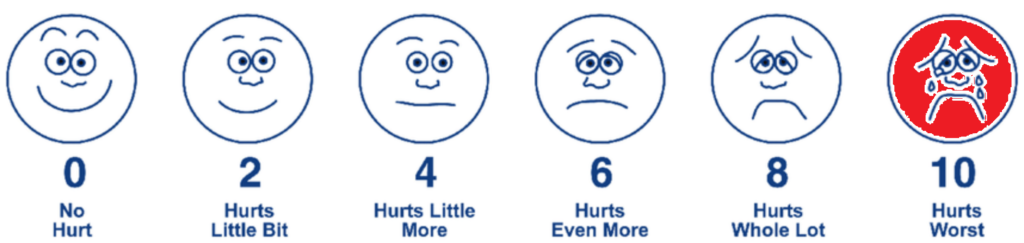
Faces Rating Scale of pain
Faces Rating Scale of pain Can be used for younger children (2-4 years). Also, work well for people with a culturally or linguistically diverse background (CALD). Ask the patient to choose the face that best describes how they feel.
Management Principles
The Nursing Management of Pain principles is:
- According to the pain scale and medication standing orders, administer paracetamol or Panadeine®
- Mild pain – Paracetamol
- Moderate pain – Panadeine or consider administration of paracetamol and ibuprofen as per standing orders dosing schedule
2. Under the following circumstances. administer ibuprofen for mild pain as an alternative to paracetamol
- Allergy or contra-indication to paracetamol.
- The patient has received 1g of paracetamol within the last 4 hours
- A patient has received 4g of paracetamol within the last 24 hours
- If the patient has associated nausea, consider administration of an antiemetic as per Standing Orders Ondansetron 4mg tablet/wafer
OR
For adult patients ≥ 20 years only, administer metoclopramide with the following considerations:
Tablet: if the patient has not vomited in the past hour and is tolerating small frequent amounts of oral fluid
Parenteral: if the patient is currently vomiting and is unable to tolerate small amounts of oral fluid
- Reassess the patient using an appropriate pain scale to assess the effectiveness of the intervention
- Document assessment findings, intervention, and outcomes.
Conclusion
Effective Nursing Management of Pain is an essential aspect of nursing care. Nurses must approach pain management from a multimodal perspective, individualizing plans for each patient, educating patients, and documenting and evaluating patient responses to interventions. By working collaboratively with patients and the healthcare team, nurses can help alleviate suffering, improve patient outcomes, and enhance overall quality of life.
