This blog post demystifies oxygen administration guidelines for nurses, equipping you with the knowledge to deliver optimal care.
Oxygen therapy is a fundamental intervention in healthcare, often used to treat patients experiencing hypoxemia. As frontline caregivers, nurses play a pivotal role in administering oxygen safely and effectively. However, ensuring proper oxygen administration requires adherence to specific guidelines and best practices. In this blog post, we’ll explore key guidelines for nurses to follow when delivering oxygen therapy to patients.
Understanding the Basics
Before delving into the guidelines, it’s essential to understand the basics of oxygen therapy. Hypoxemia, characterized by low oxygen levels in the blood, can lead to serious complications if left untreated. Oxygen therapy aims to increase the oxygen supply to tissues and organs, improving overall oxygenation and preventing further deterioration of the patient’s condition.
Oxygen Administration Guidelines for Nurses
Oxygen therapy is a crucial intervention for patients experiencing hypoxemia, but its administration requires careful consideration and specific guidelines for nurses. Incorrect administration can lead to adverse effects, highlighting the importance of understanding best practices.
Key Objectives
- Delivering Oxygen at the Appropriate Flow Rate and Concentration: One of the primary objectives of oxygen therapy is to deliver oxygen at a rate and concentration tailored to the individual patient’s needs. This requires careful assessment of the patient’s oxygen saturation levels (SpO2) and clinical condition.
- Monitoring Vital Signs: Continuous monitoring of vital signs, including SpO2, respiratory rate, heart rate, and level of consciousness, is crucial during oxygen therapy. Regular assessment allows nurses to evaluate the patient’s response to treatment and detect any signs of deterioration promptly.
- Ensuring Patient Comfort and Safety: While administering oxygen therapy, nurses must prioritize patient comfort and safety. This includes ensuring proper device application, minimizing discomfort associated with oxygen delivery, and addressing any concerns or questions the patient may have.
Assessment and Initiation
- Indications: Nurses should assess patients for signs and symptoms of hypoxemia, such as dyspnea, cyanosis, and altered mental status. Pulse oximetry readings can help determine the patient’s oxygen saturation levels, with a typical target range of 92-98% for adults.
- Order Review: Nurses must review the physician’s order for oxygen therapy, confirming the prescribed flow rate, delivery device, and target SpO2 range.
- Device Selection: Choosing the appropriate oxygen delivery device based on the patient’s needs and clinical scenario is crucial. Options include nasal cannula, simple face mask, and non-rebreather mask, among others.
Administration and Monitoring
- Setup and Application: Proper setup and secure application of the chosen oxygen delivery device are essential to ensure adequate oxygenation and patient comfort.
- Flow Rate Adjustment: Nurses should initiate oxygen therapy at the prescribed flow rate and adjust it gradually based on SpO2 readings and physician guidance.
- Continuous Monitoring: Regular monitoring of SpO2 and vital signs allows nurses to assess the patient’s response to oxygen therapy and intervene promptly if necessary.
- Patient Education: Educating patients about the purpose of oxygen therapy, proper device use, and safety precautions enhances their understanding and compliance with treatment.
Safety Considerations
- Humidification: Providing humidified oxygen, particularly for prolonged therapy, helps prevent dryness and irritation of the mucous membranes.
- Fire Risk: Nurses must keep oxygen sources and tubing away from heat sources and open flames to minimize the risk of fire. Patients and family members should also be educated about fire safety measures.
- Pressure Sores: Regular assessment of the skin under nasal prongs or mask straps helps prevent pressure sores, with repositioning as needed.
Special Populations
- Neonates and Infants: Special protocols for oxygen administration are necessary for neonates and infants due to their unique physiology and vulnerabilities.
- Patients with COPD: Nurses should exercise caution when administering oxygen to patients with chronic obstructive pulmonary disease (COPD) to avoid exacerbating respiratory distress and hypercapnia.
Conclusion
In oxygen administration guidelines for nurses conclusion, adherence to oxygen administration guidelines is paramount for nurses to ensure safe and effective therapy for patients. By delivering oxygen at the appropriate flow rate and concentration, monitoring vital signs, prioritizing patient comfort and safety, and addressing safety considerations and special populations, nurses can optimize outcomes and promote patient well-being.
Oxygen FAQs for Nurses: Breathe Easy with Confidence
What’s oxygen therapy?
It’s delivering extra oxygen to patients with low blood oxygen levels, helping them breathe easier and preventing complications.
When is oxygen therapy used?
When patients have low SpO2 (oxygen saturation) due to various conditions like pneumonia, COPD, or breathing difficulties.
How do nurses decide the oxygen therapy flow rate?
By considering SpO2 readings, the patient’s condition, and doctor’s orders. Different devices deliver varying amounts of oxygen.
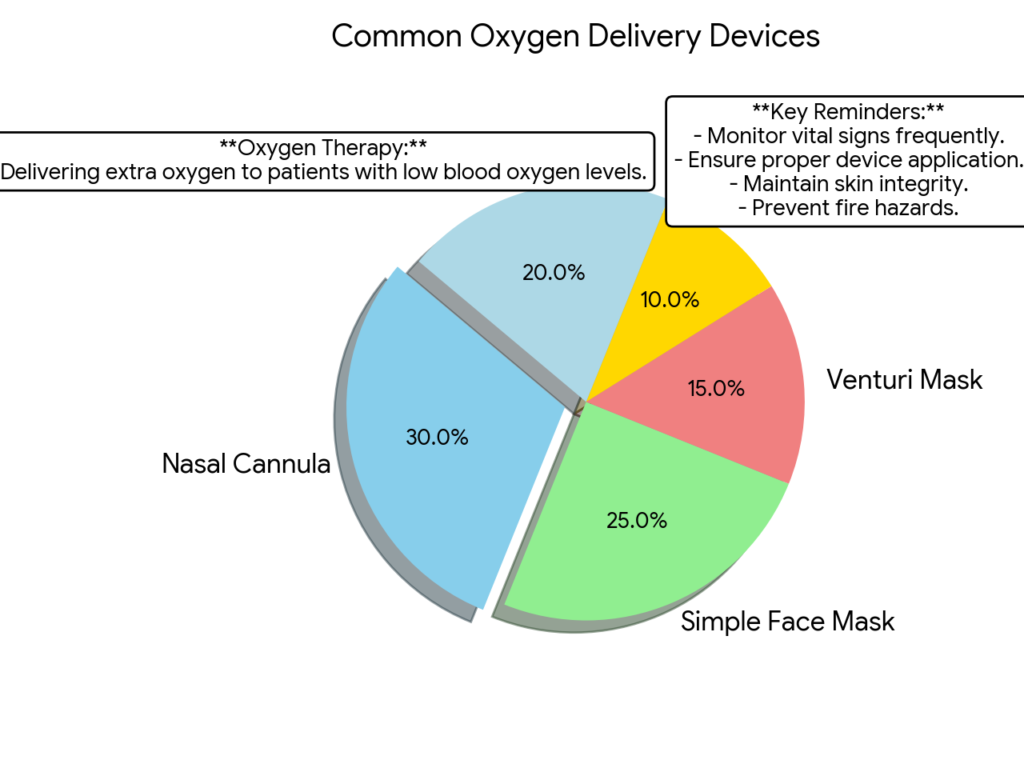
oxygen therapy Common delivery devices?
Nasal cannula, simple face mask, venturi mask, non-rebreather mask, and high-flow nasal cannula. Each has its purpose and comfort level
