In the realm of healthcare, a neurovascular assessment stands as a critical tool employed by clinicians to evaluate and diagnose potential complications related to compromised blood flow and neurological function. This systematic test is designed to identify issues early on, preventing severe consequences such as permanent injuries or, in extreme cases, loss of life.
What is a Neurovascular Assessment?
A neurovascular assessment is a comprehensive examination conducted by healthcare professionals to gauge the state of neurovascular compromise, impaired blood flow to extremities, and potential damage to peripheral nerves. This meticulous evaluation is pivotal in identifying conditions that may lead to severe consequences if not addressed promptly.
Why Perform a Neurovascular Assessment?
The rationale behind a neurovascular assessment lies in the need to detect compromised blood flow or nerve damage promptly. Such compromise can result from various factors, with compartment syndrome being a prominent concern. Compartment syndrome arises when pressure within muscles reaches hazardous levels due to internal bleeding or tissue swelling, hindering the delivery of essential nutrients to muscles and nerves. Injuries like musculoskeletal trauma, fractures, and crush injuries are common triggers, as are specific medical procedures and the application of restrictive dressings.
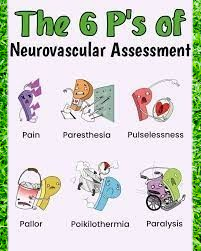
The 6 Ps of a Neurovascular Assessment
Understanding the 6 Ps of a neurovascular assessment is crucial for both clinicians and the general public. These Ps encompass pain, poikilothermia, paresthesia, paralysis, pulselessness, and pallor.
Pain
Pain, a key component of the assessment, should be localized to the site of injury. Any deviation in the expected pattern may raise suspicion of compartment syndrome.
Poikilothermia
The ability to regulate core body temperature, known as poikilothermia, is a crucial indicator. A significant temperature difference in the affected limb may signal compromised blood flow.
Paresthesia
Numbness and tingling, referred to as paresthesia, can follow an injury or surgery, signaling potential nerve damage.
Paralysis
Assessing for paralysis involves evaluating the ability to move various body parts. Clinicians test muscle strength and the capability to extend and bend limbs.
Pulselessness
The absence of pulses, particularly in the radial, dorsalis pedis, and posterior tibialis areas, signifies pulselessness. A symmetrical comparison between sides is essential.
Pallor
Pallor, indicating pale skin, may hint at compartment syndrome. Conversely, purplish or bluish discoloration may suggest poor venous return.
How to Conduct a Neurovascular Assessment
Performing a neurovascular assessment requires a systematic approach. Clinicians initiate the assessment by examining the 6 Ps, noting the location and intensity of pain, and assessing its radiation. Non-verbal cues, such as grimacing, are considered in cases where the individual cannot communicate.
Paresthesia is evaluated through light touch or the application of pressure with a pen cap. Pulse strength is graded on a scale, with a Doppler scan utilized if pulses are faint. Pallor is assessed by comparing skin color on both sides of the body, and temperature is gauged through touch. Range of motion is also tested to ensure the limbs function correctly.
Key Facts About Neurovascular Assessment
A neurovascular assessment is a pivotal diagnostic tool employed whenever there is suspicion of compromised blood flow or neurological function. This assessment revolves around the 6 Ps, including pain, poikilothermia, paresthesia, paralysis, pulselessness, and pallor. Clinicians meticulously evaluate these factors to diagnose potential issues early on, preventing severe consequences.
Purpose of Neurovascular Assessment
In clinical settings, a neurovascular assessment serves a dual purpose: identifying neurovascular compromise and assessing the circulation of blood to extremities. Additionally, it aids in the early detection of damage to peripheral nerves, ensuring timely intervention to prevent severe consequences.
When is a Neurovascular Assessment Necessary?
Clinicians initiate a neurovascular assessment whenever there’s suspicion of compromised blood flow or nerve damage. The repercussions of neurovascular compromise can be severe, making timely assessments crucial in preventing long-term damage, such as limb loss or, in extreme cases, death.
Conclusion
In conclusion, neurovascular assessments are indispensable in clinical practice. The meticulous evaluation of the 6 Ps, coupled with advanced tools and a tailored approach in special cases, ensures a comprehensive understanding of a patient’s neurovascular status. Regular assessments are key to preventing long-term complications and enhancing patient outcomes.
FAQs
How often should neurovascular assessments be performed?
Neurovascular assessments should be conducted whenever there is suspicion of compromised blood flow or nerve damage, and regularly in high-risk cases.
Are neurovascular assessments painful?
Neurovascular assessments may involve assessing pain levels, but the assessment itself is designed to be as comfortable as possible for the patient.
What is the role of technology in neurovascular assessments?
Technology, such as Doppler scans, plays a crucial role in enhancing the accuracy of pulse assessments in neurovascular evaluations.
